Since the start of the pandemic, scientists have been puzzled by the abnormal symptoms patients with the novel Coronavirus have experienced. While many Coronavirus symptoms are similar to those of the flu, others like loss of taste or smell, a dry cough, and trouble breathing have distinguished it. One of these symptoms, referred to as COVID-19 “brain fog,” causes patients to experience difficulty focusing, confusion, and, in some cases, hallucinations.
One of the largest concerns about dealing with a novel strain of the coronavirus is that scientists are still unsure about how the disease will affect those who have contracted it in the long run. According to the Mayo Clinic, while most people recover from COVID-19 after a few weeks, others, dubbed “Covid-19 long-haulers,” may experience symptoms like “brain fog” for months.
What is COVID-19 “brain fog?”
“Brain fog” isn’t a technical term, but it has been used to describe a wide array of cognitive symptoms that result from having COVID-19.
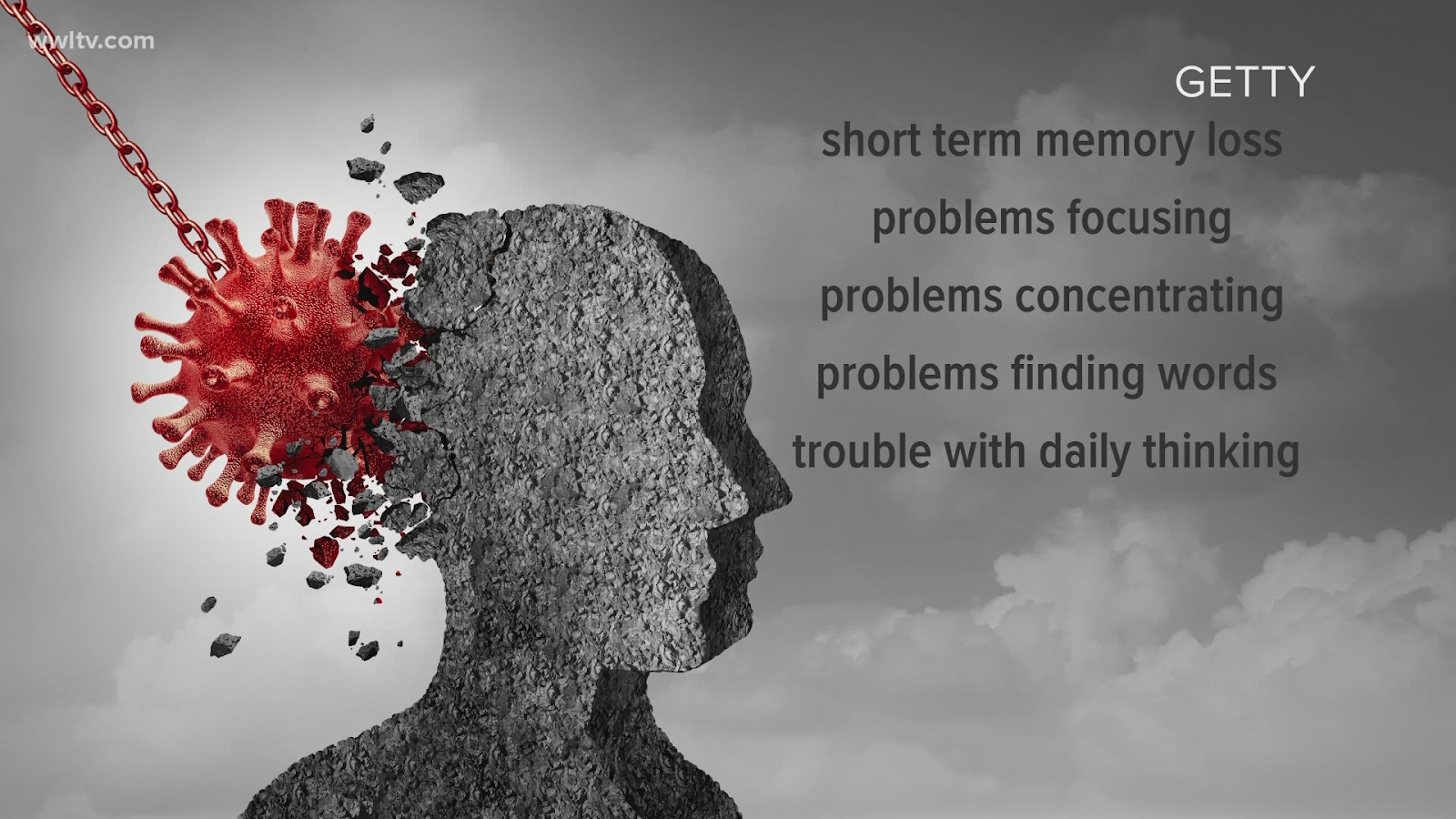
Not every one who experiences brain fog has the same cognitive symptoms, but common ones can include:
- Slow thinking
- Confusion
- Difficulty recalling words
- Trouble focusing
- Distraction
- Memory problems
- Delirium
- Psychosis
While the CDC has stated that experiencing brain fog from COVID-19 is not as common as having a fever, shortness of breath, fatigue, or coughing, it has still been reported as a long-term side effect of the virus. Brain fog is also more likely to occur from Coronavirus than it is from other viral infections.

Brain fog has been a symptom reported by people who have mild cases of COVID-19, but it is often much worse for those who have a more severe case of virus, like those who end up in the ICU. In these situations, patients are more likely to experience delirium and hallucinations. Brain fog has also been seen to affect elderly COVID-19 patients the most.
What scientists know about the causes of brain fog
Like most things regarding COVID-19, what causes patients to experience brain fog is still mostly unknown. And, according to the CDC, the effects of having long-term brain fog, while being studied, are also unknown. Generally speaking, however, it is theorized that brain fog may occur when cells in the body used to fight infections travel to places where they usually don’t reside. In the case of COVID-19 brain fog, this place is the brain.
Scientists from Johns Hopkins Medicine in Baltimore may have found evidence that suggests why brain fog is occurring in some COVID-19 patients. After conducting a study that compared the brains of those who died of COVID-19 and those who did not, researchers found that one-third of the COVID-19 brains looked at had an excessive amount of megakaryocytes in their blood vessels.
Megakaryocytes, which are usually found in bone marrow, produce platelets, tiny cell fragments found in the blood that are responsible for clotting and repairing wounds. Testing confirmed that the megakaryocytes found in the brains of COVID-19 patients seemed similar to the megakaryocytes found in bone marrow, suggesting that they originated in the bone marrow and then traveled to the brain. What makes this whole situation even more puzzling is that researchers suggest that this may be the first time that megakaryocytes have ever been found in the human brain.
As a result, scientists are perplexed about how the megakaryocytes got to the brain in the first place. It is suspected that, since COVID-19 can damage lung tissue, the megakaryocytes likely traveled from the bone marrow to the lungs and then worked their way to the brain.
But still, how they would have gotten from the lungs to the brain remains unclear, as it would mean that the large megakaryocytes would have to travel through the tiny blood vessels found in the lungs. If the megakaryocytes found in the brain didn’t come from the lungs, it’s possible that changes in the brain vessels could have trapped them there.
Regardless of how the megakaryocytes got to the brain, researchers believe that the accumulation of them could impede blood flow to the brain, affecting which areas receive oxygen. In an organ where oxygen needs to be delivered in precise locations and times, limited blood flow could create significant cognitive impairment. This would make sense as to why patients with COVID-19 are experiencing brain fog—their brain doesn’t have enough oxygen, and as a result they feel confused, distracted, and delirious.
As of right now, the actual cause of COVID-19 brain fog has not been confirmed—all researchers have right now are theories. Some scientists believe that brain fog might be caused by inflammation in the brain caused by a protein called cytokines. These proteins, which are associated with the immune system and can damage vital organs, are being found in cerebrospinal fluid (CSF), which surrounds the brain and spinal cord.
It is difficult to say what exactly is causing COVID-19 patients to experience brain fog while they have the virus, let alone months after they no longer are infected with it. There are several variables and theories at play, and researchers have not had a significant amount of time or evidence to come to a definitive conclusion, one of the setbacks of dealing with a novel coronavirus.
